Health decisions in Europe influence daily lives, long-term well-being, and social participation.
For parents, students, and professionals, making informed choices depends on access to credible information, support systems, and inclusive policy frameworks.
Decisions around vaccinations, mental health, nutrition, and access to healthcare services are rarely simple.
European Union policies, human rights instruments, and a growing focus on health literacy push institutions toward transparency and inclusiveness.
A shared goal emerges: empowering all individuals, regardless of age or professional status, to engage in meaningful health-related choices.
Children’s Rights in Healthcare Participation

Children deserve to be active contributors in decisions about their health. Involving them meaningfully fosters autonomy, builds trust, and improves health outcomes.
European health systems increasingly recognize that respecting children’s perspectives benefits everyone involved:
- Families
- Healthcare providers
- Broader communities
A structured approach to participation helps ensure that rights are upheld and responsibilities are clearly defined.
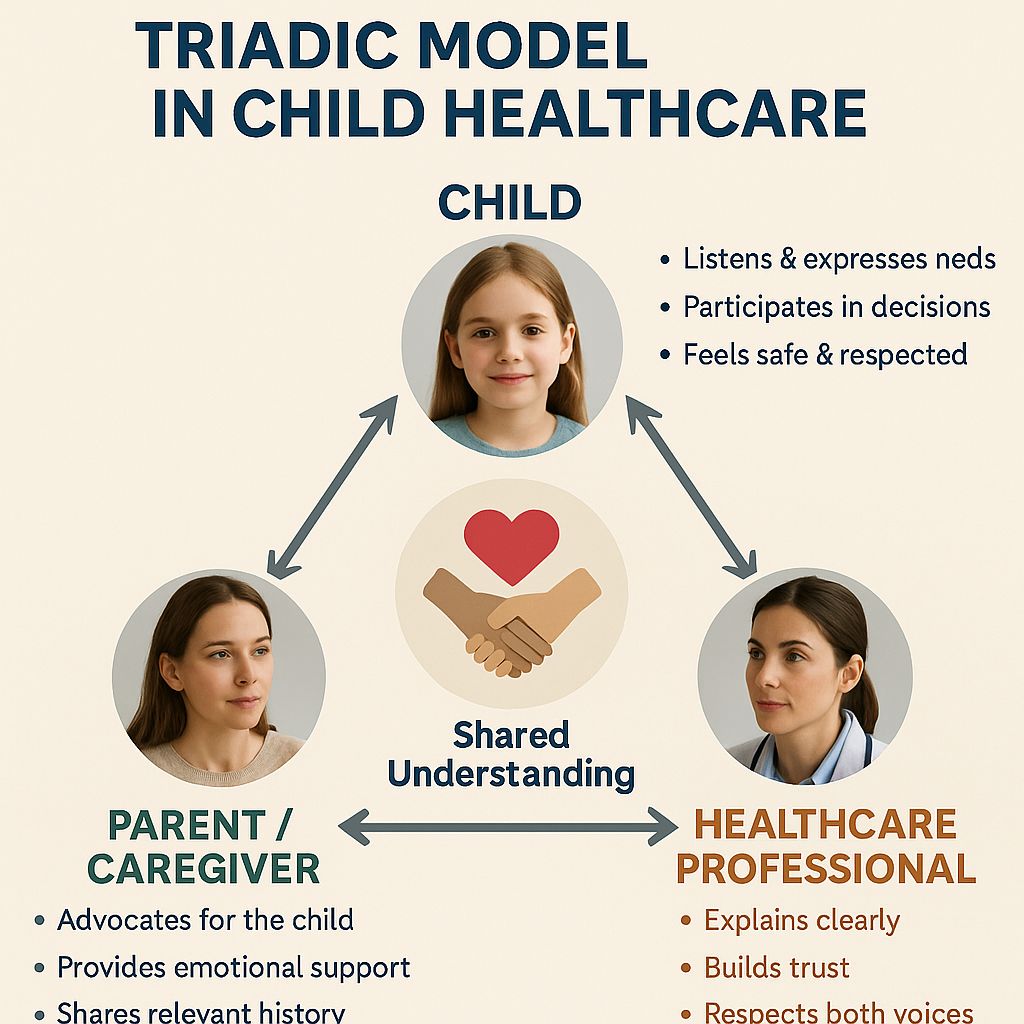
The Triadic Model in Child Healthcare

Healthcare for children is best understood as a shared enterprise between three actors: the child, the parents, and health professionals. This collaborative structure supports a balanced distribution of roles and decision-making responsibilities.
Rather than reducing children to passive patients, the model encourages active dialogue, emotional safety, and mutual accountability.
Key features of the triadic model include:
- Open, respectful communication among all three parties
- A dynamic exchange of information and feedback
- Recognition of the evolving abilities of the child
- Shared responsibility for outcomes and emotional well-being
Mutual trust forms the backbone of effective collaboration. When each participant feels respected and heard, decision-making becomes more accurate and emotionally sustainable.
The Role of Children
Children have the legal and moral right to participate in healthcare decisions. Participation must not be tokenistic.
Even younger children are capable of expressing preferences, asking questions, and offering insights into how they feel. Their input adds value and contributes to more personalized care.
To support children in healthcare decisions, professionals and parents must:
- Respect the right to be heard, regardless of age
- Encourage expression without fear of dismissal
- Offer tailored information that matches developmental stage
- Balance autonomy with protection during complex or high-risk procedures
With appropriate support, children build confidence in their ability to manage their health, which benefits them well into adulthood.
The Role of Parents
Parents carry a central role in shaping a child’s healthcare experience. Their guidance is crucial in filtering complex medical information and offering emotional reassurance.
However, the degree of control should shift gradually as children grow more capable of expressing their preferences.
Parental responsibilities include:
- Acting as emotional anchors during stressful decisions
- Explaining medical options in age-appropriate ways
- Helping children weigh risks and benefits
- Allowing room for children to form and express independent views
Factors such as culture, socio-economic status, and parental health literacy influence how effectively this role is fulfilled. More support may be needed for families facing additional pressures or barriers.
The Role of Health Professionals
Medical professionals must advocate for inclusive participation while maintaining clinical integrity.
Legal frameworks, including the UN Convention on the Rights of the Child, require that practitioners consider children’s views in treatment decisions.
Professionals promote children’s rights when they:
- Create inclusive environments where children feel safe speaking
- Use communication techniques suited to different ages
- Collaborate with parents to support child involvement
- Remain aware of power imbalances during consultations
Balancing authority with inclusivity demands training and reflexivity. Professionals who invest in these practices often find that engagement and adherence improve significantly.
Challenges in Practice
Despite the frameworks and intent, healthcare environments often fail to support genuine participation.
Structural inefficiencies, professional habits, and a lack of resources can marginalize children’s voices.
Common barriers include:
- Dominance of adult voices in consultations
- Time constraints that discourage thorough dialogue
- Inadequate training in communication with children
- Rigid protocols that overlook individuality
Improving participation requires both system-level reforms and day-to-day awareness. More time, better communication tools, and reflective practices are essential to shift this imbalance.
Structural Support via the European Child Guarantee
Health participation cannot function without the right systems in place.
Structural inequalities, socio-economic hardships, and service gaps continue to limit access for many children in Europe.
In response, the European Child Guarantee provides a policy framework designed to ensure that essential services reach those in greatest need.
Six Core Services for Children in Need
Children facing poverty or social exclusion often miss out on services that others take for granted.
The European Child Guarantee outlines six essential provisions to support their development and well-being.
The six core services include:
- Early childhood education and care
- Inclusive education and school-based activities
- One healthy meal per school day
- Access to healthcare services
- Healthy nutrition for physical and cognitive development
- Adequate housing for stability and safety
Each service plays a role in shaping a child’s trajectory, offering not just survival but the opportunity to thrive.
Education and health are tightly linked, improving one reinforces the other.
Equity Gaps in Access
Despite broad policy declarations, many children do not benefit equally. Structural and hidden barriers prevent universal access.
These inequities affect marginalized families disproportionately, especially in rural areas or underserved urban pockets.
Common obstacles include:
- Geographic disparities between urban and rural regions
- Out-of-pocket expenses for medication, school materials, or transport
- Lack of awareness or difficulty navigating local systems
- Limited access to private health insurance in low-income households
Even with public health programs, many families still encounter informal costs that limit participation. Without intentional policy action, existing disparities persist.
Policy and Practice Gaps
Commitments to child well-being require consistent follow-through. While the European Child Guarantee sets a strong direction, execution varies widely between member states.
Data gaps and ineffective monitoring contribute to sluggish implementation.
Main challenges include:
- Fragmented or outdated national databases
- Inconsistent reporting on child outcomes across regions
- Delays in allocating funding or implementing reforms
- Insufficient cooperation between local authorities and central governments
National strategies must be backed by clear metrics, transparent accountability, and adequate resources. Without these elements, service delivery remains uneven and incomplete.
Implications for Parents and Children
When children cannot access essential services, the consequences are immediate and long-lasting.
Missed medical appointments, poor nutrition, and limited school support create cascading disadvantages. These setbacks often affect entire families, not just individuals.
Consequences of limited access include:
- Worsening health conditions due to delayed or absent care
- Reduced academic performance and school attendance
- Higher stress levels in parents juggling competing demands
- Increased risk of intergenerational poverty and social exclusion
Families need predictable, affordable, and accessible support. Without it, rights remain theoretical, and opportunities stay out of reach for millions of children.
The Bottom Line

Health decisions carry weight across generations. When institutions, professionals, and families share responsibility, outcomes improve.
Europe has the tools, frameworks, and resources to foster a more participatory and equitable health environment.
Success lies in persistent collaboration and commitment to informed, inclusive action.

